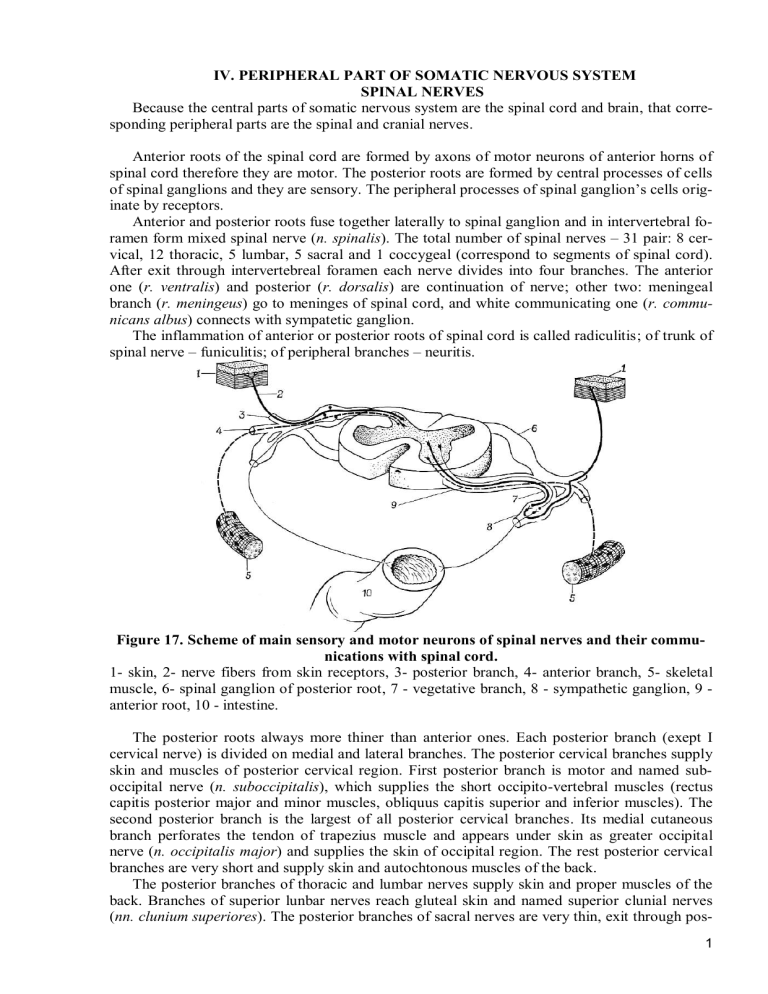
IV. PERIPHERAL PART OF SOMATIC NERVOUS SYSTEM SPINAL NERVES Because the central parts of somatic nervous system are the spinal cord and brain, that corresponding peripheral parts are the spinal and cranial nerves. Anterior roots of the spinal cord are formed by axons of motor neurons of anterior horns of spinal cord therefore they are motor. The posterior roots are formed by central processes of cells of spinal ganglions and they are sensory. The peripheral processes of spinal ganglion’s cells originate by receptors. Anterior and posterior roots fuse together laterally to spinal ganglion and in intervertebral foramen form mixed spinal nerve (n. spinalis). The total number of spinal nerves – 31 pair: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1 coccygeal (correspond to segments of spinal cord). After exit through intervertebreal foramen each nerve divides into four branches. The anterior one (r. ventralis) and posterior (r. dorsalis) are continuation of nerve; other two: meningeal branch (r. meningeus) go to meninges of spinal cord, and white communicating one (r. communicans albus) connects with sympatetic ganglion. The inflammation of anterior or posterior roots of spinal cord is called radiculitis; of trunk of spinal nerve – funiculitis; of peripheral branches – neuritis. Figure 17. Scheme of main sensory and motor neurons of spinal nerves and their communications with spinal cord. 1- skin, 2- nerve fibers from skin receptors, 3- posterior branch, 4- anterior branch, 5- skeletal muscle, 6- spinal ganglion of posterior root, 7 - vegetative branch, 8 - sympathetic ganglion, 9 anterior root, 10 - intestine. The posterior roots always more thiner than anterior ones. Each posterior branch (exept I cervical nerve) is divided on medial and lateral branches. The posterior cervical branches supply skin and muscles of posterior cervical region. First posterior branch is motor and named suboccipital nerve (n. suboccipitalis), which supplies the short occipito-vertebral muscles (rectus capitis posterior major and minor muscles, obliquus capitis superior and inferior muscles). The second posterior branch is the largest of all posterior cervical branches. Its medial cutaneous branch perforates the tendon of trapezius muscle and appears under skin as greater occipital nerve (n. occipitalis major) and supplies the skin of occipital region. The rest posterior cervical branches are very short and supply skin and autochtonous muscles of the back. The posterior branches of thoracic and lumbar nerves supply skin and proper muscles of the back. Branches of superior lunbar nerves reach gluteal skin and named superior clunial nerves (nn. clunium superiores). The posterior branches of sacral nerves are very thin, exit through pos1 terior sacral foramina and form middle clunial nerves (nn. clunium medii). The posterior branch of coccygeal nerve supplies skin over coccyx and around anus. The meningeal branches go back through intervertebral foramina to vertebral canal and supply meninges and denticulate ligament of spinal cord. They contain sensory and sympathetic fibers. The anterior branches of spinal nerves supply skin and muscles of anterior wall of body and limbs. Unlike posterior branches their fibers intertwine and form nerve plexuses. There are four large plexuses: cervical, brachial, lumbar and sacro-coccygeal. Only anterior branches of 12 thoracic nerves form no plexuses. Together with arteries and veins they pass in intercostal spaces between external and internal intercostal muscles, along lower margin of rib in costal groove and named intercostal nerves (nn. intercostales). XII intercostal nerve lies under corresponding rib and named subcostal nerve. Six upper pairs of intercostal nerves along intercostal spaces reach the sternum, and six lower ones reach anterior abdominal wall and pass between transversus abdominis and internal oblique abdominis muscles and enter rectus abdominis muscle sheath. Intercostal nerves supply deep muscles of thorax, all abdominal muscles, the skin of chest (and mammary gland) and skin of abdomen. THE CERVICAL NERVOUS PLEXUS The cervical plexus (plexus cervicalis) is formed by anterior branches of four upper cervical nerves and is located inside deep muscles of neck (prevertebral and anterior, middle and posterior scalene). The branches of this plexus are subdivided into: a) motor, b) sensory and c) mixed. The motor or muscular branches supply deep muscles of neck (rectus capitis anterior and lateralis muscles, longus capitis and colli muscles, scalene muscles). One of the motor branches inferior root, radix inferior, crosses externally internal jugular vein and fuses with superior root of hypoglossal nerve, forming the ansa cervicalis. Its branches supply infrahyoid muscles of neck (the sternohyoid, sternothyroid, thyrohyoid and omohyoid). The sensory branches of cervical plexus go out between superior and middle thirds of posterior margin of sternocleidomastoid muscle. They supply the skin of neck, occiput and chest in infraclavicular region. The branches are: – the lesser occipital nerve (n. occipitalis minor) – along the posterior margin of sternocleidomastoid muscle it goes upwards and supplies the skin of occipital region. – the greater auricular nerve (n. auricularis magnus) – the largest cutaneous branch. It goes upwards to auricle along external surface of sternocleidomastoid and supplies the skin of external acoustic meatus and convex part of auricule and the skin of parotideomasseteric region. – the transverse cervical nerve (n. transversus colli) – cross transversely the sternocleidomastoid muscle and gives 4 branches. The upperst of them fuses with ramus colli of facial nerve. It supplies the skin of anterior region of neck. – the supraclavicular nerves (nn. supraclaviculares) descend and supply the skin above the clavicle and pectoralis major and deltoid muscles. The mixed branches: phrenic nerve (n. phrenicus) – the longest nerve of cervical plexus. It descends in front of the anterior scalenus muscle, enters thoracic cavity: the left one crosses anteriorly aortic arch, the right goes externally to superior vena cava. Both go down to diaphragm in front of roots of lungs on lateral surface of heart between pericardium and mediastinal pleura. Its motor fibers supply the muscular part of diaphragm. The sensory ones – the mediastinal pleura, pericardium and going through caval opening of diaphragm in abdominal cavity, supply a fibrous capsule of liver and its ligaments. The phrenicus sign – Tenderness after pressing between crura of sternocleidomastoid muscle above right clavicle. Pain radiates to liver area. It is positive in case of liver or gallbladder diseases. THE BRACHIAL PLEXSUS 2 The brachial plexus (plexus brachialis) is formed by anterior branches of the four lower cervical nerves and the major part of first thoracic nerve (С5-С8, Th1). Conditionally the brachial plexus is divided into supraclavicular and infraclavicular parts. First one is located in spatium interscalenum above subclavian artery as three trunks: superior, middle and inferior. Second one is in the axillary cavity and represented by 3 cords: the medial, lateral and posterior, which surround the axillary artery. Branches of brachial plexus are classified as short and long. The short branches originate from supraclavicular part. Conditionally they are divided into two groups: 1) nerves to scapula: dorsal scapular nerve (n. dorsalis scapulae) – it supplies levator scapulae muscle; suprascapular nerve (n. suprascapularis) with the same name artery supplies supraspinatus and infraspinatus muscles; subscapular nerves (nn. subscapulares) – by 2-3 branches supplies subscapular and teres major muscles; 2) nerves thorax: the medial and lateral pectoral nerves (nn. pectorales medialis et lateralis) supply the pectoralis major and minor muscles; the long thoracic nerve (n. thoracicus longus) – it goes at external surface of serratus anterior muscle and supplies it; the thoracodorsal nerve (n. thoracodorsalis) – it goes along the lateral margin of scapula and supplies the latissimus dorsi muscle. And the thinest nerve of short branches – the subclavian nerve (n. subclavius) goes in front of subclavian artery more laterally to phrenic nerve and supplies subclavius muscle. Figure 18. The cervical and brachial plexuses. The long branches originate from infraclavicular part. The branches of medial cord: – the medial root of median nerve; – the medial cutaneous brachial nerve (n. cutaneus brachii medialis) – it supplies the skin of corresponding region; 3 – the medial cutaneous antebrachial nerve (n. cutaneus antebrachii medialis) – it supplies corresponding skin; – the ulnar nerve (n. ulnaris), which is mixed. The ulnar nerve gives no branches on arm, but goes through medial bicipital groove together with median nerve and brachial artery, and then behind medial humeral epicondyle and in forearm goes through ulnar groove together with ulnar artery. It supplies the flexor carpi ulnaris and medial half of flexor digitorum profundus muscles. Than on palm it is divided on deep (muscular) and superficial (sensory) branches. It supplies skin around V and medial half of IV finger (1.5 fingers), dorsal skin of 2.5 fingers (V, IV medial half of III) and majority muscles of hand. The branches of lateral cord: – the lateral root o median nerve; – the musculocutaneus nerve (n. musculocutaneus) – it supplies the anterior group of brachial muscles, its continuation lateral cutaneous antebrachial nerve (n. cutaneus antebrachii lateralis) – skin of this region. The median nerve (n. medianus) – mixed, it originates by two roots from lateral and medial cords. It gives no branches for the arm, goes through medial bicipital groove, median groove of forearm and supplies all anterior muscles of the forearm except flexor carpi ulnaris and medial half of flexor digitorum profundus muscles. Through the carpal canal under retinaculum flexorum it enters the palm and is divided on common digital nerves. It supplies partly thenar muscles, I and II lumbrical muscles as well as and skin of 3.5 fingers (I, II, III and lateral half of IV). From posterior cord: – the axillary nerve (n. axillaris), it is thick and short (sometimes considered as short branch of brachial plexus), it goes back through foramen quadrilaterum of posterior wall of axillary cavity. Its terminal branch is the superior lateral cutaneous brachial nerve. Its muscular branches supply to the deltoid and teres minor muscles. – the radial nerve (n. radialis) – the thickest branch of brachial plexus. It goes back through humeromuscular canal together with deep brachial artery and veins. In cubital fossa it is divided into superficial and deep branches. It supplies posterior group of arm and forearm muscles. Its sensory branches supply skin of posterior side of arm, forearm and hand of 2.5 fingers (I, II and lateral half of III). In such case it is named like «the king» of all posterior part of upper limb. The abbreviation “UMRU” for marking of zones of skin innervations of hand and fingers: on palm 1.5 fingers supplied by Ulnar nerve and 3.5 – Median, on the dorsal side laterally 2.5 – the Radial and 2.5 – Ulnar one. But the skin of distal phalanges of fingers is supplied similar to palmar side: the medial 1.5 fingers by ulnar nerve, 3.5 fingers – by median nerve. THE LUMBAR PLEXUS. SACROCOCCYGEAL PLEXUS Common lumbosacral plexus (pl. lumbosacralis) is formed by all anterior branches of lumbar, sacral and coccigeal nerves according zones of innervation are subdivided on two plexuses: the lumbar and sacrococcygeal. The lumbar plexus (pl. lumbalis) is formed by anterior branches of XII thoracic (partially), I, II, III, IV (partially) lumbar spinal nerves. The muscular branches (rr. musculares) supply quadratus lumborum, psoas major and minor muscles. Iliohypogastric nerve (n. iliohypogastricus) lies on quadratus lumborum muscle parallel to ХII intercostal nerve. Then it goes between transverse and internal oblique abdominis muscles, ending in hypogastric region. It supplies anterior abdominal wall, and by anterior and posterior branches supply the skin of suprapubic region and skin above the trochanter major. Ilioinguinal nerve (n. ilioinguinalis) goes between abdominal muscles, but its cutaneous branch - through inguinal canal and supplies to the skin of scrotum (or labia majora). The lateral cutaneous femoral nerve (n. cutaneus femoris lateralis) goes under inguinal ligament and supplies the lateral surface of skin of thigh. The genitofemoral nerve (n. genitofemoralis) is located at anterior surface the psoas major muscle and separates on two branches: a) the genital (r. genitalis), which goes through inguinal 4 canal and supplies to m. cremaster and skin of scrotum (in males), the round ligament of uterus and skin of labia majora (in females); b) femoral (r. femorails), which goes through vascular lacuna and supplies the skin of thigh below inguinal ligament. The largest branches of the plexus are the femoral and obturator ones. The femoral nerve (n. femoralis) reach the thigh under inguinal ligament through the muscular lacuna together with iliopsoas muscle. At the thigh it divides at the following brunches: the muscular (to iliopsoas, quadriceps femoris, sartorius and pectineus muscles); the anterior cutaneus femoral nerve and saphenous nerve (n. saphenus). The last one goes together with femoral artery and femoral vein in adductor (Hunter’s) canal, descends on medial surface of leg around the medial malleus and enters medial surface of foot and supple skin of these areas. The obturator nerve (n. obturatorius) leaves lumbar plexus medially to psoas major muscle, descends to lesser pelvis, on its lateral wall reaches the obturator canal. Through it goes at medial surface of the thigh and supplies the medial group of muscles and skin of medial surface of inferior part of the thigh and hip joint. Figure 19. The lumbar and sacral plexus. 1 – n. subcostalis. 2 – n. iliohypogastricus. 3 – n. ilioinguinalis. 4 – truncus lumbosacralis. 5 – n. cutaneus femoris lateralis. 6 – n. genitofemoralis. 7 – n. femoralis. 8 – n. obturatorius. 9 – pl. sacralis. 10 – gangl. sympatica sacralia. 11 – truncus sympathicus. 12 – pl. aorticus abdominalis. The sacral plexus (pl. sacralis) – the largest of plexuses and is formed by anterior branches of IV (partially) and V lumbar, all sacral spinal nerves. It lies inside lesser pelvis on piriformis muscle. Its branches exit pelvic cavity through supra- and infrapiriform foramina to gluteal region. The branches of this plexus are subdivided at short and long ones. The short branches: a) muscular – supply piriformis, internal obturatorius, gemelli superior and inferior as well as quadratus femoris muscles; b) superior gluteal nerve (n. gluteus superior) – goes through suprapiriform foramen and supplies to gluteus medius and minimus and tensor fasciae latae muscles; b) the inferior gluteal nerve (n. gluteus inferior) – exits through infrapiriform foramen and supplies the gluteus maximus muscle; c) the pudendal nerve (n. pudendus) – goes out with inferior gluteal nerve, surrounds sciatic spine and through the lesser sciatic foramen goes back to the pelvis, into ischiorectal faoosa, where it divides into the terminal branches: 5 the inferior rectal (nn. rectales inferiores) – supply external anal sphincter and skin around anal canal; perineal nerves (nn. perineales) – to skin and muscles of perineum; the posterior scrotal or posterior labial (nn. scrotales s. labiales posteriores) supply to the skin of posterior part of scrotum and labia majora; the dorsal nerve of penis or clitoris (n. dorsalis penis s. clitoridis) give branches to corresponding organs and contain large number of vegetative fibers. The long branches of sacral plexus: the posterior cutaneous femoral nerve and sciatic nerve. The posterior cutaneous femoral nerve (n. cutaneus femoris posterior) – sensory, enters thigh under inferior margin of gluteus maximus muscle and supplies the skin of inferior part of buttocks (nn. clunium inferiores), perineum, posterior surface of thigh, popliteal fossa. The sciatic nerve (n. ischiadicus) is mixed. It is the largest nerve of human body. It goes out through infrapiriform foramen, in gluteal region it lies under gluteus maximus muscle. Near its inferior margin nerve is located just under fascia lata (the place of most variable damage of it). At the thigh it goes between muscles of posterior group and supplies to them. In popliteal fossa the sciatic nerve divides into tibial and common peroneal nerves. The tibial nerve (n. tibialis). In poplitael fossa it gives off the medial sural cutaneous nerve (n. cutaneus surae medialis), after that it goes within cruropoliteal canal together with posterior tibial artery and veins. Then it travels behind in the medial malleolus, goes to plantar surface of foot and divides into terminal branches - the medial and lateral plantar nerve. Besides, tibial nerve gives off also: muscular (to posterior muscles of leg) and articular branches (to knee and talocrural joints). The medial sural cutaneous nerve (n. cutaneus surae medialis) goes between heads of gastrocnemius muscle and joins with the lateral sural cutaneous nerve, forming the sural nerve (n. suralis), which behind the lateral malleolus continuous as the lateral dorsal cutaneous nerve (n. cutaneus dorsalis lateralis), which supplies the lateral part of foot. On the leg medial sural cutaneous nerve supplies to the skin of posterior-medial surface. The medial plantar nerve supplies to the flexor digitorum brevis muscle, I and II lumbrical muscles and the plantar skin of medial 3.5 toes. The lateral plantar nerve supplies to the rest of plantar muscles and the skin of the rest 1.5 toes and lateral half of the plantar surface. Common peroneal nerve (n. peroneus (fibularis) communis) passes forwards around the neck of the fibula within the substance of peroneus (fibularis) longus, where it terminates by dividing into the superficial and deep peroneal (fibular) nerves. Before this, common peroneal nerve gives off the lateral sural cutaneous nerve (n. cutaneus surae lateralis), supplying to the skin of posterior-lateral surface of leg, and it joins the medial sural cutaneous nerve to form sural nerve. The superficial peroneal nerve (n. peroneus (fibularis) superficialis) goes down inside musculoperoneal canal between fibula and origin of peroneal muscles, which it supplies), it continuous at dorsum of foot by two nerves: the medial and intermediate dorsal cutaneous nerves (n. cutaneus dorsalis medialis et intermedius). They supply the skin of dorsal side of foot, except first interdigital space. The deep peroneal nerve (n. peroneus (fibularis) profundus) moves together with anterior tibial artery and veins between anterior muscles of leg and supplies to them. It gives off branches to talocrural joint and dorsal muscles of foot and skin of first interdigital space. So, the sciatic nerve and its branches supply to posterior muscles of thigh, all muscles of leg and foot, skin of leg (except the medial surface) and foot (except the medial margin of dorsal side). The coccygeal plexus is created by V lumbar and coccygeal spinal nerves – it supplies the skin over the coccyx. 6 CRANIAL NERVES Cranial nerves, nn. craniales, are nerves that are anatomically and functionally connected to the brain. There are 12 pairs of cranial nerves, which are indicated by Roman digits: I pair - olfactory nerves, nn. olfactorii; II pair - optic nerve, n. opticus; III pair - oculomotor nerve, n. oculomotorius; IV pair - trochlear nerve, n. trochlearis; V pair - trigeminal nerve, n. trigeminus; VI pair - abducent nerve, n. abducens; VII pair - facial nerve, n. facialis; VIII pair - vestibulocochlear nerve, n. vestibulocochlearis; IX pair - glossopharyngeal nerve, n. glossopharyngeus; X pair - vagus nerve, n. vagus; XI pair - accessory nerve, n. accessorius; XII pair - hypoglossal nerve, n. hypoglossus; Fig. 20. Internal surface of base of the skull with cranial nerves. I and II pairs of cranial nerves are derived from the forebrain, III-XII pairs are related to various parts of the brainstem. III and IV pairs are connected with the midbrain, V-VIII - with the pons, and IX-XII - with the medulla oblongata. According to the composition of the fibers, cranial nerves are divided into 3 groups: 1) sensory nerves - I, II and VIII pairs; 2) motor nerves - IV, VI, XI and XII pairs; 7 3) mixed nerves - III, V, VII, IX and X pairs (taking into account that the parasympathetic part of the III nerve innervates exclusively muscles, this pair is also sometimes referred to as motor nerves). Sensory nerves are formed by centripetal fibers (central processes) of cells located in the nasal mucosa for the I pair, in the retina for the II pair or in the sensory ganglion of the VIII pair. The motor nerves are formed by axons of cells of the motor nuclei of the cranial nerves IV, VI, XI and XII pairs. Mixed nerves have different fiber composition. The sensory component present in V, VII, IX, and X pairs of cranial nerves is represented by central processes of pseudounipolar cells located in sensory ganglions. The motor component present in III-VII, IX-XII pairs of cranial nerves is represented by axons of cells of the motor nuclei of the corresponding nerves. The parasympathetic component in the mixed nerves is found in III, VII, IX and X pairs of cranial nerves. It is formed by preganglionic parasympathetic fibers extending from the parasympathetic nuclei of the corresponding nerves to the autonomic ganglia or postganglionic fibers, which are axons of the cells of these ganglions. The name, localization of the autonomic ganglions and nerves containing parasympathetic fibers are indicated in the table (see below). It should be noted that in the composition of the motor and mixed cranial nerves there are also sympathetic postganglionic fibers originating from the superior cervical ganglion of the sympathetic trunk. PHILO- AND ONTOGENESIS OF CRANIAL NERVES Phylogenetically the cranial nerves lost their initial segmental location and became highly specialized. The olfactory and optic nerves are specific nerves of the sensory organs that develop from the forebrain and are its outgrowths. They connect the organ of smell and the organ of vision to the brain. The rest of cranial nerves are derived from the spinal nerves and are fundamentally similar to them. The III pair (oculomotor nerve), the fourth pair (trochlear nerve) and the VI pair (abducent nerve) developed in connection with the preauricular myotomes, innervates the muscles of the eyeball that developed from these myotomes. These nerves, as well as the XI and XII pairs, are similar to the anterior roots of the spinal nerves. V, VII, VIII, IX and X pairs of cranial nerves are homologues of the posterior roots. These nerves are associated with muscles developing from the muscles of the branchial apparatus and developed from the lateral plates of the mesoderm, therefore they innervate the skin, muscles of the corresponding visceral branchial arches, and also contain visceral motor fibers, innervating glands and organs of the head and neck. A special place is occupied by the V pair (trigeminal nerve), which is formed by the fusion of two nerves - the deep optic nerve, innervating the skin of the anterior surface of the head, and the trigeminal nerve itself, innervating the skin and muscles of the mandibular arch. In development, the VIII pair (vestibulocochlear nerve) is separated from the facial nerve, which carries out the specific innervation of the organ of hearing and balance. IX pair (glossopharyngeal nerve) and X pair (vagus nerve), which consists of visceral motor nerve fibers, develop by isolating the caudal part of the vagus nerve. The hypoglossal nerve is complex in origin, as it is formed by the fusion of few spinal nerves, some of which move cranially and enter the region of the medulla oblongata. Thus, all 12 pairs of cranial nerves by origin can be divided into several groups: 1. Nerves - derivatives of the brain - I (n. olfactorius) and II pairs (n. opticus). 2. Nerves developing in connection with the head myotomes - III (n. oculomotorius), IV (n. trochlearis), VI (n. abducent) pairs. 3. Nerves - derivatives of branchial arches - V (n. trigeminus), VII (n. facialis), VIII (n. vestibulocochlearis), IX (n. glossopharyngeus), X (n. vagus), XI (n. accessorius) pairs. 4. The nerve that developed by the fusion of the spinal nerves - XII pair (n. hypoglossus). 8 The cranial nerves, like the spinal nerves, have nuclei (accumulations of gray matter): somatic sensory (corresponding to the posterior horns of the gray matter of the spinal cord), somatic motor (corresponding to the anterior horns) and vegetative (corresponding to the lateral horns). Vegetative can be divided into visceral motor and visceral sensory, moreover, visceral motor not only innervate unstriated (smooth) muscles, but also provide trophics to skeletal muscles. Given that the striated muscles received the features of somatic muscles, all the nuclei of the cranial nerves related to such muscles are better designated as somatic motor. As a result, the composition of the cranial nerves contains the same components as in the spinal nerves. Afferent components: 1) somatic sensory fibers coming from organs that perceive physical stimuli (pressure, pain, temperature, sound and light) i.e. skin, organs of hearing and vision - II, V, VIII. 2) visceral sensory fibers coming from organs that perceive internal stimuli, i.e. from nerve endings in the digestive organs and other viscera, from the special organs of the pharynx, oral (gustatory organ) and nasal (olfactory organ) cavities - I, V, VII, IX, X. Efferent components: 1) somatic motor fibers innervating voluntary muscles, namely: muscles originating from head myotomes, eye muscles (III, IV, VI), sublingual muscles (XII), and skeletal muscles that are secondarily displaced into the anterior digestive tract - the so-called muscles of the branchial apparatus, which have become masticatory, facial, etc. in mammals and humans. (V, VII, IX, X, XI); 2) visceral motor vegetative fibers (parasympathetic and sympathetic fibers) innervating visceral muscles, i.e. involuntary muscles of blood vessels and internal organs, muscle of the heart, as well as various glands (secretory fibers), - V, VII, IX, X. Scheme for the studying and description of cranial nerves 1. Numbering and name of the nerve (English, Latin). 2. Functional characteristic (motor, sensory, mixed). 3. Source of nerve development. 4. Nerve nuclei (name, functional characteristic, topography). 5. The principle of nerve formation, sensory ganglions. 6. Place of entry (sensory) or exit (motor, parasympathetic) of nerves from the brain. 7. The place of entry or exit of nerves from the skull. 8. The passage of the nerve in the periphery. 9. Parasympathetic ganglions associated with nerves. 10. The main trunks and branches of the nerve, their area of innervation. SENSORY GANGLIONS OF CRANIAL NERVES AND THEIR LOCALIZATION Name of nerve and number of pair Name of ganglion Trigeminal nerve, n. trigeminus, V pair Ganglion trigeminale Localization of ganglion Facial nerve, n. facialis, VII pair Ganglion geniculi Vestibulocochlear nerve, n. vestibulocochlearis, VIII pair Glossopharyngeal nerve, n. glossopharyngeus, IX pair Vagus nerve, n. vagus, X pair Ganglion vestibulare, ganglion cochleare Ganglion superius, ganglion inferius Trigeminal impression of anterior surface of temporal pyramid Geniculum of facial canal in temporal pyramid Floor of internal acoustic meatus, spiral canal of cochlear modiolus Jugular foramen, fossula petrosa Ganglion superius, ganglion inferius Jugular foramen, below to it CRANIAL NERVES 9 Name of nerve and number of pair I., nn. olfactorii (S) Sourse of development Nuclei and their topography derivatives of the forebrain — II. n. opticus (S) derivatives of the — forebrain III. n. oculomoto- Derivatives of the Nucleus n. oculomotorii rius (M, P) head myotomes (M). Tegmentum mesencephali, level of superior colliculi Nucleus accessorius (P) and unpaired median (P). the same place as previous one, somewhat medially and posteriorly IV. n. trochlearis Derivatives of the Nucleusn. trochlearis (M) (M) head myotomes Tegmentum mesencephali, level of inferior colliculi Place of exiting Place of exiting from cranial from brain or enInnervated organs cavity or entertering in it ing in it Bulbus olfactorius Lamina cribro- Regio olfactoria musa ossis eth- cosa of nasal cavity moidalis Chiasma opticum Sulcus Fissura orbitaloculomotorius, is superior fossa interpeduncularis Posteriorly to the tegmentum of the midbrain. Pass around cerebral peduncles V. n. trigeminus Homologues of Nucleus motorius n. Anteriorly the mid(M, S) the posterior roots trigemini (M). In superior dle cerebellar peof spinal nerves. part pars dorsalis pontis duncle (anterior Derivatives of part of linea tribranchial arches gemino-facialis) Nucleus pontinus n. trigemini (S). laterally to the previous one Nucleus spinalis n. trigemini (S). Continuation of the previous one along all medulla oblongata. Nucleus tractus mesencephalici n. trigemini (S). In the tegmentum of the midbrain, laterally to the aqueduct. VI. n. abducens Derivatives of the Nucleus n. abducentis (M) head myotomes (M). Dorsal part of pons, in the area of colliculus facialis VII. n. facialis (n. Homologues of Nucleus n. facialis (M) intermedius) (M, S, the posterior roots Dorsal part of pons, forP) of spinal nerves. matio reticularis Derivatives of branchial arches Nucleus solitarius (S). Dorsal part of pons Nucleus salivatorius superior (P) Formatio reticularis, pars dorsalis pontis (posteriorly to nucleus of facial nerve) 10 Canalis opticus Retina of eyeball М. Levator palpebrae superioris, m. rectus medialis, m. rectus superior, m. rectus inferior, m. obliquus inferior M. ciliaris, m. sphincter pupillae Fissura orbital- M. obliqus superior is superior N. ophthalmicus – fissura orbi-talis superior, n. maxillaris – foramen rotun-dum, n. mandibularis – foramen ovale (M) Mm. masticatores, m. tensor veli palatini, m. tensor tympani, m. mylohyoideus, venter anterior m. digastrici (S) Skin of frontal and temporal regions, skin of face. (S) Mucosa of nasal and oral cavities, anterior 2\3 of the tongue, teeth, salivary glands, organs and tissues of orbit, dura matter of anterior and middle cranial fossa Posterior edge of Fissura orbital- M. rectus lateralis pons, in the groove is superior between pons and pyramid. Posteriorly to mid- Porus acusticus (M) Mm. faciales, m. dle cerebellar pe- internus – cana- platysma, venter duncle (posterior lis facialis – posterior m. digapart of linea tri- foramen stylo- strici, m. stуlohygeminofacialis) mastoideum oideus, m. stapedius (S) gustatory sense of anterior 2/3 of the tongue (P) Glandula lacrimalis, tunica mucosa oris, tunica mucosa nasi (glands), gl. sublingualis, gl. submandibularis, glandulae salivatoria minores VIII. n. Homologues vestibulocochlearis of the posterior (S) roots of spinal nerves. Pars cochlearis Derivatives of Pars vestibularis branchial arches IX., n. glossophaHomologues ryngeus (M, S, P) of the posterior roots of spinal nerves. Derivatives of branchial arches X. n. vagus (M, S, Homologues of P) the posterior roots of spinal nerves. Derivatives of branchial arches XI. n. accessorius Homologues of (M) the posterior roots of spinal nerves. Derivatives of branchial arches In the region of lateral angle of rhomboid fossa (area vestibularis) Nuclei cochleares ventralis et dorsalis (S) Nuclei vestibulares medialis, lateralis, superior et inferior (S) Nucleus solitarius (S) Doraslly in the medulla oblongata, in the region of trigonum n. vagi as a continuation of this nucleus Nucleus salivatorius inferior (P) In formatio reticularis of medulla oblongata between nucleus ambiguus and olivary nucleus. Nucleus ambiguus (M) Formatio reticularis of medulla oblongata Nucleus solitarius (S) In the region of trigonum n. vagi, in medulla oblongata. Ponto-cerebellar angle Porus acusticus Organon spirale, internus crista ampulares, macula utriculi, macula sacculi Inferiorly to two Foramen jugu- (S) Cavum tympani, previous ones in lare tuba auditiva, tunica superior part of mucosa radicis linsulcus dorsolatguae, pharyngis, toneralis, posteriorly silla palatina, glomus to olive caroticus, glandula parotidea (M) M. stylopharyngeus. Muscles of pharynx The same groove Foramen (S) Dura mater of the as n. glossopha- jugulare posterior cranial fossa, ryngeus caudally to skin of internal acoustic it meatus. Organs of the neck, thorax and abdomen (except left part of large intestine) Nucleusdorsalisn.vagi (P) (P) Smooth muscles and in the same area, dorsally glands of organs of thoto the previous one racic and abdominal cavities (except left part of large intestine) Nucleus ambiguus (M). (M) Tunica muscularis Formatio reticularis medulpharyngis, m. levator veli la oblongata, deeper to nupalatini, m. uvulae, m. cleus dorsalis n. vagi palatoglossus, m. palatopharyngeus, mm. laryngis Nucleus ambiguus (M) Radices craniales Foramen jugu- М. sternocleidoIn medulla oblongata as a the same groove as lare mastoideus, m. tracontinuation of the same n. vagus, but more pezius name nucleus of X, XI caudally. pairs Nucleus spinalis n. accessorii (M). In between anterior and posterior horns of the spinal cord Radices spinales between anterior and posterior roots of the cervical nerves on the level С2-C6 segments XII. n. hypoglosHomologues Nucleus n. hypoglossi Sulcus Canalis n. hy- Muscles of the tongue sus (M) of the anterior (M). In medulla oblongata ventrolateralis of poglossi roots of spinal in the region of trigonum medulla oblongata nerves. nervi hypoglossi Примечание: (M) – motor innervation (S) – sensory innervation (P) – parasympatetic innervation 11 Fig. 21. Areas of innervations of cranial nerves (scheme). I PAIR – OLFACTORY NERVES, NERVI OLFACTORII. OLFACTORY PATH These are nerves of special sense - they consist of visceral sensory fibers (perceive chemical irritation - odors). Unlike other cranial sensory nerves, the olfactory nerve does not have a sensory nucleus or ganglion. Therefore, they are called false cranial nerves. The first neuron is located on the periphery in regio olfactoria of the mucous membrane of the nasal cavity (superior nasal concha and upper part of the nasal septum). The dendrites of the olfactory cells are directed to the free surface of the mucous membrane, where they end with the olfactory vesicles, and the axons form the olfactory filaments, fili olfactorii, 15-20 on each side, which penetrate into the cranial cavity through the cribriform plate of the ethmoid bone. In the cranial cavity, they reach the olfactory bulbs of the lower surface of the frontal lobe of the cerebral hemispheres and end there. The second neurons are located in the olfactory bulbs, the axons of which form the olfactory tract, tractus olfactorius. This tract goes along the lower surface of the frontal lobe 12 in the groove of the same name and ends in the olfactory triangle, anterior perforated substance and a septum pellucidum, where the third neurons of the olfactory path are located. Axons of the third neurons are divided into two bands: 1. The lateral stria, stria lateralis, goes on its side to the cortex of uncus, giving part of the fibers to the amygdaloid body. 2. The medial stria, stria medialis, goes to another hemisphere. Its fibers pass through the anterior commissure of the brain, continuing on the opposite side in the form of a diagonal stria (stria diagonalis, seu bandaletta diagonalis, Broca's diagonal band). As a result, the fibers reach the same centers as the previous ones (uncus, amygdaloid body), but on the contralateral (opposite) side. An intermediate stria, stria intermedia, which goes to the mammilary bodies (corpora mamillaria), is also determined. From neurons of the mammilary bodies begins the mammillothalamic fasciculus, fasciculus mamillothalamicus. This tract is the beginning of the Papetz cycle. Among the pathologies of the olfactory analyzer are known such as: anosmia - complete loss of smell (possible unilateral and bilateral anosmia), hyposmia - reduced ability to smell, dysosmia - perverted perception of smells, phantosmia - perception of nonexistent odors. The causes of these pathologies can be extremely diverse: congenital disorders, injuries, infection, inflammatory processes of the brain, toxic processes, neurodegenerative diseases, etc. II PAIR – OPTIC NERVE, NERVUS OPTICUS. Like the olfactory nerves, it belongs to the false cranial nerves, has no ganglion and nucleus. It is a nerve of special sense (light) and consists of fibers, which are a set of axons of multipolar ganglionic cells of the retina. The optic nerve begins with the optic disc in the area of the optic part of the retina, its blind spot. Perforating the vascular and fibrous tunics, it leaves the eyeball medially and inferiorly from its posterior pole. In accordance with the topography there are four parts of the optic nerve: - intraocular, perforating choroid and sclera of the eyeball; - orbital, extending from the eyeball to the optic canal; - intracanalicular, corresponding to the length of the optic canal; - intracranial, located in the subarachnoid space of the base of the brain, extending from the optic canal to the optic chiasm. In the orbit, the optic canal and in the cranial cavity the optic nerve is surrounded by a sheath (vagina), the layers of which correspond to the meninges of the brain, and the intravaginal spaces correspond to the intermeningeal spaces. The first three neurons are in the retina. The set of photosensitive retinal cells (rods and cones) are the first neurons of the optic tract; giant and small bipolar cells - the second neuron; multipolar ganglionic cells - the third neuron. The axons of these cells form the optic nerve. The nerve passes through the optic canal, canalis opticus, and enters the cranial cavity. In the area of the prechiasmatic groove 2/3 of all nerve fibers coming from the medial visual fields decussate. These fibers come from the medial parts of the retina, which receives visual information from the lateral sides due to the intersection of light beams in the lens. Approximately 1/3 nondecussating fibers go into the optic tract of their side. They come from the lateral parts of the retina, which receives light from the nasal half of the visual field (lens effect). An incomplete decussation of the optic tracts allows the transmission of impulses from each eye to both hemispheres, providing binocular stereoscopic vision and the possibility of synchronous movement of the eyeballs. After this partial decussation optic tracts are formed and bend around the cerebral peduncles from the lateral side and appear on the dorsal part of the brainstem. Each optic tract contains fibers from the same retinal halves of both eyes. So, in the composition of the right optic tract, non-crossed fibers from the lateral half of the right eye and crossed fibers from the medial half of the left eye pass. Therefore, the right optic tract conducts a nerve impulse from the 13 lateral part of the visual field of the left eye and the medial (nasal) part of the visual field of the right eye. The fibers of each optic tract follow in 3 directions that pass to the subcortical visual centers: - lateral geniculate bodies of the diencephalon, corpora geniculate lateralis; - pulvinar of the thalamus of the diencephalon, pulvinar thalami (then to the cortex); and part of the fibers, without synapse in geniculate bodies, follows through the brachium into - superior colliculi of the tectum of the midbrain, colliculi superioris tecti mesencephalici. The main subcortical center of vision is the lateral geniculate bodies, where most of the fibers of the optic path end. Here its fourth neurons are located. The axons of these neurons in a compact bundle pass through the posterior third of the posterior limb of the internal capsule, then form optic radiation, radiation optica, and end on neurons of the cortical center of vision on the medial surface of the occipital lobe on the sides of the calcarine sulcus. A small number of fibers of the optic tracts are directed to the neurons of the posterior nuclei of the thalamus. The axons of the neurons of these nuclei transmit visual information to the integration center of the diencephalon - the medial nucleus of the thalamus, which has connections with the motor nuclei of the extrapyramidal and limbic systems. These structures regulate muscle tone, carry out emotional-behavioral reactions, and alter the functioning of internal organs in response to visual irritations. A part of the fibers goes to the superior colliculi, providing an unconditionally reflex reaction of the eyeball and the implementation of the pupil reflex in response to light irritations. The axons of the nucleus of the superior colliculi are directed to the motor nuclei of the III, IV, VI pairs of cranial nerves, to the accessory nucleus of the oculomotor nerve (the nucleus of K. Westphal, L. Edinger), to the nuclei of the reticular formation, to the nucleus of Cajal’s and to the integration center of the midbrain, which is also located in the superior colliculi. The connections of the neurons of the superior colliculi with the motor nuclei of III, IV, VI pairs of cranial nerves provide a motor reaction of the eyeball muscles to light stimuli (binocular vision) and connections with the neurons of the Cajal’s nucleus allows coordinated movement of the eyeballs and head (maintaining body balance). From the cells of the integration center of the midbrain begins the tecto-spinal and tecto-nuclear tracts, which carry out unconditional reflex motor reactions of the muscles of the trunk, limbs, head and eyeballs to sudden strong light irritations. From the cells of the reticular formation, the reticulopetal and reticulospinal tracts begin, which regulating muscle tone in conjunction with exogenous irritations. The cells of the accessory nucleus of the oculomotor nerve send axons to the ciliary ganglion, which provides parasympathetic innervation of the sphincter pupillae muscle and ciliary muscle, which provides accommodation for the eye. The chain of neurons providing these reactions is called the pathway of pupil reflex. The pathway of the pupil light reflex It provides an involuntary response of the pupil to light. It consists of two parts: sensory and motor. The sensory one is part of the optic nerve and contains four neurons (the first three are in the retina, the fourth is in the superior colliculi of the quadrigeminal plate). The processes of the fourth neurons are directed to the parasympathetic nucleus of Yakubovich, where the fifth neuron of the pupil light reflex pathway is located and its motor part begins, which is part of the oculomotor nerve. Together with the oculomotor nerve, the processes of the fifth neuron enter the orbit through the superior orbital fissure. Here the parasympathetic fibers are separated, forming the so-called parasympathetic root of the ciliary ganglion, radix parasympathica ganglion ciliare, enter this parasympathetic ganglion and end on its cells, which are the sixth neurons of the pupil light reflex pathway. Axons of sixth neurons are sent to the eyeball and innervate the ciliary muscle, m. сiliaris and sphincter pupillae muscle, m. sphincter pupillae. 14 The examination of visual fields is very important for neurological practice. The loss of half of the visual fields is called hemianopsia. In case of complete blockage of the optic nerve, blindness occurs in this eye - amaurosis. With partial damage to the fibers of the optic nerve, there are limitations of the visual fields in the form of a sector or island - scotoma of the affected eye. In case of total destroying of optic chiasm, there is complete bilateral blindness, anopsia. With partial damage to the optic chiasm (pituitary tumors, hydrocephalus), when pressure affects the fibers coming from the inner halves of the retina of both eyes, bitemporal hemianopsia occurs, i.e. the right eye falls out in one eye, and the left field of vision in the other. If the outer corners of the optic chiasm are damaged (due to carotid aneurysm), the lesion will affect the temporal halves of both retinas. In case of damage to the optic tract, lateral geniculate bodies, thalamus, and occipital lobe, hemianopsia is observed, i.e. loss of opposite visual fields. When examining the fundus of the eyeball, attention should be paid to the change in the nipple of the optic nerve with an increase in intracranial pressure (congestive nipple), its atrophy in pituitary tumors. Hypertension is characterized by the phenomenon of narrowing of arteries and dilation of veins. III PAIR – OCULOMOTOR NERVE, NERVUS OCULOMOTORIUS This is a mixed nerve somatic animal and autonomic parasympathetic fibers. It has 2 nuclei: motor, nucleus nervi oculomotorii, and parasympathetic, accessory nucleus (Yakubovich or Edinger-Westphal), nucleus accessorius. The nuclei are located in the tegmentum of the midbrain at the level of the superior colliculi of the quadrigeminal plate. The nerve exits from the brain in the interpeduncular (Tarin’s fossa), fossa interpeduncularis. After leaving the brain, the nerve enters the cavernous sinus, sinus cavernosus, and exits the skull through the superior orbital fissure, fissura orbitalis superior, entering the orbit. Here it is divided into 2 branches: superior and inferior, ramus superior et inferior. The superior branch goes along the upper wall of the orbit and innervates levator palpebrae superioris muscle and the superior rectus muscle of the eyeball, m. levator palpebre superior et m. rectus superior. The inferior one goes along the lower wall of the orbit, gives off the parasympathetic root of the ciliary ganglion. These parasympathetic fibers after synapse in the ciliary ganglion (see the pathway of the pupil light reflex) innervate the smooth muscles of the eyeball. The remaining fibers of the inferior branch are divided into three bundles and innervate the medial and inferior rectus muscles of the eyeball and the inferior oblique muscle of the eyeball. With complete damage to the oculomotor nerve, the following pathology is observed: 1. Due to a violation of the innervation of the levator palpebrae superioris muscle, the eye is covered with a drooped eyelid - ptosis. 2. The eyeball is turned outward and slightly downward (due to the preserved action on the eye muscles of the branches IV and V of the pairs of cranial nerves). 3. The pupil is dilated (due to preserved action of the dilator pupillae muscle). 4. Deterioration of vision at short distances due to paralysis of accommodation (ciliary muscle is affected). 5. The inability to move the eyeball up and inward due to damage to the superior and medial rectus muscles of the eyeball. IV PAIR – TROCHLEAR NERVE, NERVUS TROCHLEARIS Motor nerve. It has one motor nucleus, nucl. nervi trochlearis, which lies in the lining of the midbrain at the level of the inferior colliculi of the quadrigeminal plate. It exits the midbrain from the dorsal surface after the decussation of its fibers in the superior medullary velum, velum medullare superius. The nerve pass laterally to the cerebral peduncles, appear on the inferior surface of the brain, perforate the dura mater, passes into the cavernous sinus along with the oculomotor and ophtalmic nerves. It exits the skull through the superior orbital fissure, fissura orbitalis superior. It goes along the upper wall of the orbit and innervates the superior oblique muscle of the eyeball, m. obliquus superior. 15 Injury to trochlear nerve causes convergent strabismus and diplopia (double vision when looking down). V PAIR – TRIGEMINAL NERVE, NERVUS TRIGEMINUS. PARASYMPATHIC GANGLIONS OF THE HEAD Mixed nerve, contains motor and sensory fibers. The first neuron of the sensory part is located in the trigeminal (semilunar, Gasserian) ganglion, ganglion trigeminale seu semilunare, located on the anterior surface of the temporal bone pyramid, in the trigeminal impression. Here, the dura mater splits into two layers, forming the Meckel’s cave, in which the trigeminal ganglion is located. The peripheral processes of the cells located in the ganglion go to the periphery, forming three branches of the trigeminal nerve, and the central ones, forming a sensory root, radix sensoria, enter the brainstem, where they end on three sensory nuclei: spinal nucleus of trigeminal nerve, n. spinalis nervi trigemini (projected onto the rhomboid fossa, descending to the spinal cord), mesencephalic nucleus of trigeminal nerve, n. mesencephalicus nervi trigemini, which rises up into the midbrain, and the principal sensory (pontine) nucleus, n. principalis nervi trigemini. The motor part of the trigeminal nerve starts from one motor nucleus, n. motorius nervi trigemini, the processes of which, leaving the brain, form the motor root, radix motoria, which passes under the Gasserian ganglion and join the third branch of the trigeminal nerve. Thus, the first branch of the trigeminal nerve is the ophtalmic nerve, n. ophthalmicus, is fully sensory, the second branch is maxillary, n. maxillaris, also sensory, and the third - the mandibular nerve, n. mandibularis contains both sensory and motor fibers. A feature of the trigeminal nerve is the presence of the autonomic cranial ganglions along its branches. Cells of these ganglions receive the preganglionic parasympathetic fibers from the nuclei of the III, VII and IX pairs of cranial nerves. Postganglionic fibers attach to the branches of the trigeminal nerve and reach the working organ. Each branch of the trigeminal nerve gives the meningeal branch, r. meningeus, to the dura mater of the brain. Ophtalmic nerve, nervus ophthalmicus The first branch of the trigeminal nerve. It carries out the sensory innervation of the eyeball, lacrimal gland, lacrimal sac, mucous membrane of the ethmoid labyrinth, frontal and sphenoid sinuses, skin and conjunctiva of the upper eyelid, glabella, nose, forehead. Therefore, its innervation zone is located above the palpebral fissure. Sensory nerve. It starts from the Gasserian ganglion, passes through the lateral wall of the cavernous sinus. Exiting the cavernous sinus, it gives a branch to the cerebellum, r. tentorii, goes into the orbit through the superior orbital fissure and divides into 3 nerves: 1. Nasociliary nerve, n. nasociliaris. 2. Frontal nerve, n. frontalis. 3. Lacrimal nerve, n. lacrimalis. 1. Nasociliary nerve, n. nasociliaris, goes along the medial wall of the orbit to the medial corner of the eyeball and gives off 5 branches: - sensory root of ciliary ganglion, radix sensoria ganglii ciliaris - goes to the ciliary ganglion; - long ciliary nerves, nn. ciliares longi - innervate the tunics of the eyeball; - posterior ethmoidal nerve, n. ethmoidalis posterior, - enters the nasal cavity through the foramen with the same name and innervates the mucous membrane of the nasal cavity and sphenoid sinus; - anterior ethmoidal nerve, n. ethmoidalis anterior, - goes into the cranial cavity through the foramen with the same name, and then through the cribriform plate, penetrates the nasal cavity, gives a branch to the frontal sinus and innervates the anterior sections of the lateral wall and nasal septum, up to the tip of the nose; 16 - infratrochlear nerve, n. infratrochlearis, - is the terminal branch of the nasociliary nerve. It goes to the medial corner of the eye, where it anastomoses with the supratrochlear nerve. 2. The frontal nerve, n. frontalis, goes along the superior wall of the orbit and divides into three nerves: - supratrochlear nerve, n. supratrochlearis, - anastomoses with the infratrochlear nerve and they innervate the skin and conjunctiva of the medial corner of the eye, the lacrimal sac, the skin of the dorsum of the nose and forehead; - supraorbital nerve, n. supraorbitalis, - innervates the skin of the forehead and scalp; - the frontal branch, r. frontalis - goes to the frontal region and innervates the skin of this area. 3. The lacrimal nerve, n. lacrimalis, goes along the lateral wall of the orbit, where an anastomosis from the zygomatic nerve, ramus communicans cum nervo zygomatico, approaches it. This anastomosis consists of vegetative fibers coming from the pterygopalatine ganglion. The nerve becomes mixed (contains sensory, sympathetic and parasympathetic fibers). The lacrimal branches, rr. lаcrimale, with all vegetative fibers and part of the sensory ones innervate the lacrimal gland, and the lacrimal nerve, in which only the sensory fibers remained, innervates the skin and conjunctiva of the lateral angle of the eye. Along the first branch of the trigeminal nerve is the ciliary ganglion, ganglion ciliare, which is in the orbital cavity. Ciliary ganglion, ganglion ciliare The parasympathetic vegetative ganglion is located in the orbit laterally to the optic nerve. Three types of fibers are suitable for it: 1. Parasympathetic root, radix parasympathica, parasympathetic fibers that come from the nucleus of Yakubovich as part of the oculomotor nerve. 2. Sensory root, radix sensoria, - sensory fibers coming from the nasociliary nerve. 3. Sympathetic root, radix sympathica, - sympathetic fibers coming from the cavernous plexus. Since the ganglion is parasympathetic and contains only parasympathetic cells, parasympathetic fibers are interrupted (i.e., the transmission of a nerve impulse through synaptic connections to the nerve cells of the ganglion), while sensory and sympathetic fibers transit. Three types of fibers form 3-6 short ciliary nerves, nn. ciliares breves: - parasympathetic - innervate the sphincter pupillae muscle, m. sphincter pupillae; - sympathetic - dilator pupillae muscle, m. dilatator pupillae; - sensory - innervate the nucleus of the eyeball. Maxillary nerve, nervus maxillaris The second branch of the trigeminal nerve innervates the gums and teeth of maxilla, nose, lower eyelid, upper lip, cheek and temporal region, mucous membrane of the palate, upper lip, nasal cavity, maxillary sinus, cheek. Therefore, it innervates the middle part of the face between the palpebral fissure and the angle of the mouth. Sensory nerve begins in the Gasserian ganglion. It leaves the skull through foramen rotundum. Before exiting the skull, the meningeal branch, ramus meningeus, which innervates the dura matter of the middle cranial fossa, departs from it. Leaving the skull, the nerve enters the pterygopalatine fossa, fossa pterygopalatina, where it is divided into three branches: 1. Ganglionic branches, rr. ganglionares. 2. Zygomatic nerve, n. zygomaticus. 3. Infraorbital nerve, n. infraorbitalis. 1. Ganglionic branches, rr. ganglionares, pass to the pterygopalatine ganglion, ganglion pterygopalatinum. Using these branches, a mutual exchange of fibers between the nerve and the ganglion is carried out, that’s why all branches of the nerve and the ganglion will include sensory, sympathetic and parasympathetic components. 17 2. Zygomatic nerve, n. zygomaticus, leaves the pterygopalatine fossa through the inferior orbital fissure, enters the orbit, goes along its lateral wall, where it gives the connecting branch to the lacrimal nerve ramus communicans cum nervo lacrimalo. Then, through the zygomaticoorbital foramen, foramen zygomaticoorbitale, goes inside the zygomatic bone, where it is divided into two branches: - zygomaticofacial, r. zygomaticofacialis, which, through the foramen with the same name, leaves the zygomatic bone and innervates the skin of the lateral surface of the face; - zygomaticotemporal, r. zygomaticotemporalis, which goes through the foramen with the same name and innervates the skin of the temporal region. 3. Infraorbital nerve, n. infraorbitalis, through the inferior orbital fissure enters the orbital cavity, goes along its inferior wall, enters the infraorbital groove and canal and through the infraorbital foramen, foramen infraorbitalis, enters the face, where it divides into its terminal branches. Inside the pterygopalatine fossa, the posterior superior alveolar branches, rr. alveolares superiores posteriores through the foramens with the same name enter the maxilla and participate in the formation of the superior dental plexus, plexus dentalis superior, from which the dental branches innervate molars. In the region of the infraorbital groove and canal, the superior middle and anterior alveolar branches, rr. alveolares superior medius et anteriores, also participate in formation of superior dental plexus which giving tooth branches, rr. dentales superiores to premolars, incisors and canines and superior gingival branches, rr. gingivales superius. Plexuses located in the alveolar process of the maxilla exchange fibers, which explains the irradiation of pain in dental diseases. When entering the face through the infraorbital foramen in the canine fossa, the nerve forms a "small goose foot", pes anserinus minor, consisting of branches that innervate: - skin of the lower eyelid, rami palpebrales inferiores; - skin of the lateral surface of the nose, rami nasales externi; - skin and mucous membranes of the upper lip and gums, rami labiales superiores; - the mucous membrane of the anterior sections of the nasal cavity, rr. nasales inferiores. Pterygopalatine ganglion, g. pterygopalatinum This is a parasympathetic (paraorganic, third order) ganglion, located in the adipose tissue of the pterygopalatine fossa. Three types of fibers are suitable for it: 1. Sensory root, radix sensoria, - ganglionic branches, rr. ganglionares, from the maxillary nerve. 2. Parasympathetic root, radix parasympathiсa, is a greater petrosal nerve, n. petrosus major, which extends from the intermediate nerve (VII pair) along the anterior surface of the temporal bone pyramid to the foramen lacerum. 3. Sympathetic root, radix sympathiсa, is a deep petrosal nerve, n. petrosus profundus, which begins from the internal carotid plexus, plexus caroticus internus, formed by neurons of the superior cervical ganglion of the sympathetic trunk. Sympathetic and parasympathetic roots i.e. the greater and deep petrosal nerves are connected in the region of foramen lacerum, forming a pterygoid, or Vidian nerve, n. canalis pterygoidei, which enters the pterygopalatine fossa through the channel of the same name and reaches the pterygopalatine ganglion. Since it is a parasympathetic ganglion, only parasympathetic fibers are interrupted in it, while sensory and sympathetic ones transit. From the ganglion arise: - medial and lateral superior posterior nasal branches, rr. nasales posteriores superiores mediales et laterales, which penetrate the sphenopalatine foramen and pass to the mucous membrane of the posterior sections of the superior and middle nasal meatuses; - inferior posterior nasal branches, rr. nasales posteriores inferiores, traveling through the greater palatine canal to the mucous membrane of the floor of the nasal cavity; 18 - nasopalatine nerve, n. nasopalatinus, (Scapra’s nerve), passing first through the sphenopalatine foramen to the mucous membrane of the nasal septum, and then through the incisive canal, canalis incisivus, to the mucous membrane of the hard and soft palate; - greater and lesser palatine nerves, nn. palatini major et minor; from the pterygopalatine fossa go through the canals with the same name enters the oral cavity, where innervates the mucous membrane of the hard and soft palate. Mandibular nerve, nervus mandibularis The third branch of the trigeminal nerve innervates the gums and teeth of the lower jaw, the mucous membrane of the tongue, cheek and lower lip, skin of chin, submandibular and sublingual salivary glands, temporo-mandibular joint, mastication muscles, some muscles of the neck, palate and middle ear. Therefore, the sensory fibers of this nerve innervate the lower part of the face (below the angle of the mouth). This is a mixed nerve that contains both sensory and motor fibers. Sensory fibers start from the Gasserian ganglion, and motor fibers start from the motor nucleus, nucleus motorius. It leaves the skull through the foramen ovale, and enters the infratemporal fossa, fossa infratemporalis. Immediately after exiting the skull, the spinosus nerve (or meningeal branch), n. spinosus departs from it, which returns through foramen spinosum to the cranial cavity and innervates the dura mater of the middle cranial fossa. In the infratemporal fossa, the nerve is divided into two branches: 1. The anterior, ramus anterior, mainly motor, to the mastication muscles. 2. The posterior, ramus posterior, mostly sensory. From the anterior branch arise: 1.1. The masseteric nerve to the masetter muscle, n. massetericus. 1.2. Deep temporal nerves, nn. temporales profundi, to the temporal muscle. 1.3. Lateral pterygoid nerve, n. pterygoideus lateralis, to the muscle of the same name. These three nerves are motor, and the fourth: 1.4. The buccal nerve, n. buccalis, is a sensory, innervating skin and mucosa of cheek. From the posterior branch: 2.1. Medial pterygoid nerve, n. pterygoideus medialis, motor, innervate the muscle with the same name, and also give branches to tensor veli palatine muscle and tensor tympani muscle, m. tensor veli palatini et m. tensor tympani. 2.2. Lingual nerve, n. lingualis, sensory, passes between the pterygoid muscles, then goes down and anteriorly along the inner surface of the lower jaw, enters the tongue and ends there. The chorda tympani, which is a branch of the VII pair of cranial nerves, carries parasympathetic fibers and fibers of taste sense, attaches to the lingual nerve. In addition, sympathetic fibers from the external carotid plexus, plexus caroticus externus, (its continuation is the facial plexus, plexus facialis) are suitable for the lingual nerve. Thus, the nerve becomes mixed and contains 4 types of fibers: general sensory, special sensory (taste), parasympathetic and sympathetic fibers. From the lingual nerve depart: - sublingual nerve, n. sublingualis, contain three types of fibers, except taste. Firstly pass to the sublingual ganglion, ganglion sublinguale. After the ganglion all three types of fibers are sent to the sublingual salivary gland. - submandibular branches, rr. submandibulare, contain three types of fibers, except taste. Firstly sent to the node with the same name, ganglion submandibulare, and then to the submandibular salivary gland. - lingual branches, rr. linguales, contain all 4 types of fibers. Fibers of general sense innervate the anterior two-thirds of the tongue, fibers of taste sense innervate all the papillae of the tongue except the vallate, and vegetative fibers innervate the small salivary glands of the tongue. - branches to isthmus of fauces, rr. isthmi faucimi, to the mucous membrane of the palato-glossal arch and to the palatine tonsils. 19 Submandibular, g. submandibulare, and sublingual ganglions, g. sublingvale Located next to the glands of the same name, parasympathetic in structure, containing peripheral parasympathetic neurons whose axons (postganglionic fibers) end in the salivary glands of the tongue, submandibular and sublingual glands. Preganglionic parasympathetic fibers extend from the superior salivary nucleus of the facial nerve. They pass as a component of chorda tympani, lingual and submandibular nerves of the mandibular nerve and are interrupted on the neurons of the ganglions. General sensory fibers are called ganglionic branches, rami ganglionares. After passing through ganglions, they provide general sensation to these glands. Sympathetic fibers enter the ganglions from the plexus of the lingual artery, pl. sympathicus a. lingualis, transit through ganglions and bring trophic innervation. 2.3. Inferior alveolar nerve, n. alveolaris inferior, a mixed nerve, contains sensory and motor fibers. It goes along the inner surface of the lower jaw and in the region of mandibular foramen is divided into sensory and motor parts. Sensory fibers enter the mandibular canal and exit through the mental foramen. Inside the canal nerve gives inferior alveolar branches, rr. alveolares inferiores, which enter the alveolar process of the lower jaw, form the plexus, plexus dentalis inferior, from which the branches to lower tooth arise, rr. dentales inferiores, and the inferior gingival branches, rr. gingivales inferiores. The terminal branch of the sensory part, n. mentalis, innervates the skin of the chin and mucous membrane of the lower lip. Motor fibers form the mylohyoid nerve, n. mylohyoideus, which goes along the inner surface of the lower jaw in the groove of the same name and innervates the muscle of the same name and the anterior belly of the digastric muscle, m. digastricus. 2.4. Auriculotemporal nerve, n. auriculotemporalis, sensory, goes in front of external acoustic meatus up to the temporal region. The branches from the otic ganglion attaches to it. Otic ganglion, g.oticum It is located on the base of the skull near the foramen ovale. Parasympathetic ganglion (paraorganic, III order, terminal). Three types of fibers are suitable for it: 1. Sensory - connecting branches from the mandibular nerve, rr. communicans cum g. oticum. 2. Parasympathetic fibers - a lesser petrosal nerve, n. petrosus minor, which is a branch of IX pair. 3. Sympathetic fibers come from the plexus of the middle meningeal artery, pехus a. meningeus medius, which is part of the external carotid plexus. Parasympathetic fibers in the node are interrupted, while sensory and sympathetic fibers transit. All three types of fibers join the auriculotemporal nerve. The nerve gives groups of branches: - articular, rami articulares - sensory, innervate the temporo-mandibular joint; - nerves of the external acoustic meatus, nn. meatus acustici externi – sensory, innervates the skin of the external acoustic meatus; - anteriorauricular nerves, nn. auriculares anteriores – sensory, innervate skin and cartilage of the anterior auricle; - superficial temporal branches, rr. temporalis superficiales – sensory, to the skin of the temporal region; - branches of the tympanic membrane, rr. membranae tympani, to the eardrum; - parotid branches, rr. parotidei - contain three types of fibers and innervate the parotid salivary gland, glandula parotis. Damage to one of the branches of the trigeminal nerve causes disturbance of all types of sensation in the innervation zone. The reflexes associated with this nerve either depressed or lost. In case of damage to the motor root of this nerve, paralysis of the masticatory muscles develops. With one-sided damage, the lower jaw deviates toward the damage when opening the mouth, bilateral paralysis makes it impossible to chew and leads to sagging of the lower jaw. Damaging of the nucleus of the spinal tract of the trigeminal nerve leads to dissociated anesthesia or hyper20 esthesia (only pain and temperature sensitivity are disturbed). Lesions of the trigeminal nerve are usually accompanied by disorders of sweating, vasomotor phenomena, disorders of tissue nutrition, which are especially dangerous in the cornea (neurotrophic keratitis), dysfunction of large glands of the oral cavity. VEGETATIVE (PARASYMPATHETIC) CRANIAL GANGLIONS Name of ganglion Ganglion ciliare Ganglion pterygopalatinum Parasympathetic center of brainstem; nerves with preganglionic parasympathetic fibers Orbita, laterally Nucl. accesorius n.opticus n.оculomotorii, radix oculоmоtorius from n. oculomotоrius Fossa pterygоpala- Nucl. salivatorius superitina along n. or, nucl. lacrimalis, n. maxillaris petrosus from n. facialis Localization of ganglion Ganglion submandibulare Glandula submandibularis superiorly Ganglion sublinguale Glandula submandibularis superiorly Ganglion oticum Basis cranii externa under foramen ovale along n. mandibularis Nerves with postganglionic parasympatheric fibers Target organ Nn. ciliares breves M. sphincter pupillae, m. ciliaris Nn. palatini, nn. nasales posteriores,n. zygomaticus Nucl. salivatorius Rr. submandibulasuperior, chorda tympani res from n. facialis Nucl. salivatorius Rr. sublinguales superior, chorda tympani from n. facialis Nucl. salivatorius inferior, N. auriculotemn. petrosus minor from n. poralis glosopharyngeus Mucosa of palate, nasal cavity, lacrimal gland Glandula submandibularis Glandula sublingualis Glandula parotidea VI PAIR - ABDUCENT NERVE, NERVUS ABDUCENS This is a motor nerve. It has one motor nucleus, nucleus nervi abducentis, which is located in the pons and is projected in the upper triangle of the rhomboid fossa (in the region of the facial colliculus, colliculus facialis). It comes out of the brain between the pons and the pyramid of the medulla oblongata. Then the nerve passes anteriorly through the medial wall of the cavernous sinus (together with the internal carotid artery). Enters the orbit through the superior orbital fissure and innervates the lateral rectus muscle of the eyeball, m. rectus lateralis. When a nerve is damaged, a convergent strabismus, the inability to turn the eyeball outward, diplopia when looking towards the damaged muscle are noted. VII PAIR - FACIAL NERVE, NERVUS FACIALIS The mixed nerve contains sensory, motor and parasympathetic fibers. Motor fibers are axons of the motor nucleus, nucl. nervi facialis located in the depths of the pons under the facial colliculus. Sensory fibers are a collection of peripheral processes of pseudounipolar cells of the sensory geniculate ganglion, ganglion geniculi. The central processes end on the neurons of the nucleus of solitary tract, nucl. tractus solitarius. The preganglionic parasympathetic fibers of the facial nerve begin from the parasympathetic nucleus of pontine tegmentum - the superior salivary, nucl. salivatorius superior. Sensory and secretory fibers are combined under the name of the intermediate nerve, n. intermedius, and the motor part of the fibers is proper facial nerve, n. facialis proprius. Proper facial nerve, nervus facialis proprius The motor, has one motor nucleus, which is located in the pons and is projected in the upper triangle of the rhomboid fossa, the fibers go into the colliculus facialis, form a loop and exit the brain between the pons and the medulla oblongata in the pontocerebellar angle. Then the 21 nerve goes to the back of the pyramid and through porus acoustics internus enters meatus acousticus internus and facial canal. In the facial canal, the nerve runs horizontally, going outwards, then turns at a right angle backwards, after that it descends vertically, exiting the skull through stylomastoid foramen. Upon leaving the skull, the nerve bends forward, enters the parotid gland, in the thickness of which forms the parotid plexus, plexus parotideus, and divides into terminal branches. On its way, the nerve gives 9 branches: 1. Stapedius nerve, n. stapedius, departs in the facial canal and innervates the stapedius muscle. 2. Posterior auricular nerve, n. auricularis posterior, after leaving the facial canal innervates the muscles of the auricle and the occipital belly of the cranial muscle, venter occipitalis m. epicranii. 3. Digastric branch, ramus digastricus, innervates the posterior belly of m. digastricus. 4. Stylohyoid branch, ramus stylohyoideus, to the muscle of the same name. The terminal five branches form pes anserinus major, and innervate all the muscles of facial expression and platysma. These nerves go anterior to the auricle of the tragus, radially splitting into the terminal branches. Therefore, vertical sections on the face are not recommended. 5. Temporal branches, rami temporales, innervate mm. auricularis anterior, orbicularis oculi, epicranius (venter frontalis), corrugator supercilii, procerus. 6. Zygomatic branches, rami zygomatici, innervate m.m. zygomatici et orbicularis oculi. 7. Buccal branches, rami buccales, innervate mm. risorius, buccalis, levator labii superioris, orbicularis oris, levator anguli oris et nasales. 8. Marginal branch, ramus marginalis mandibulae, - goes along the edge of the lower jaw to the chin, innervates mm. depressor labii inferiores, mentalis, depressor anguli oris. 9. Cervical branch, ramus coli, runs down behind the angle of the lower jaw and innervates platysma, forming with the transverse nerve of the neck from the cervical plexus a superficial cervical loop, ansa cervicalis superficialis. Intermediate nerve, n. intermedius The nerve is mixed, contains parasympathetic fibers and sensory (special sense (taste)) fibers. It has two nuclei projected onto the rhomboid fossa: - parasympathetic superior salivary nucleus, nucleus salivatorius superior; - the sensory nucleus of solitary tract, nucleus tractus solitarii, common to the VII, IX and X pairs. The fibers go along with the facial nerve and enter the facial canal. In the area of geniculum canalis facialis, there is a peripheral sensory ganglion, ganglion geniculi, which consists of pseudounipolar cells, the peripheral processes of which go to the organs, and the central ones go to the brain, to the nucleus of solitary tract. After this ganglion two nerves are formed: 1. The greater petrosal nerve, n. petrosus major, - consists of parasympathetic preganglionic fibers. It leaves the canal of the temporal bone through hiatus canalis nervi petrosi majoris on the anterior surface of the pyramid, lies in the groove of the same name, reaches foramen lacerum, where it joins deep petrosal nerve, n. petrosus profundus, forming the Vidian nerve or nerve of pterygoid canal, n. canalis pterygoidei. Through the pterygoid canal this nerve enters the pterygopalatine fossa and reaches the ganglion of the same name, where it preganglionic fibers interconnect. From the ganglion, vegetative fibers reach n. maxillaris, then pass to n. zygomaticus, and as a component of the communicating branches depart to the lacrimal nerve and in the form of rr. lacrimales are sent to the lacrimal gland, which they innervate. 2. The chorda tympani, consists of sensory gustatory and parasympathetic preganglionic fibers. It passes in the facial canal, then enters the tympanic cavity through its posterior wall, passes between the malleus and the incus, and exits the tympanic cavity through a petrotympanic (Glaserian) fissure, fissure petrotympanica. Then it goes down between the pterygoid muscles and joins the lingual nerve. Parasympathetic fibers of the chorda tympani, after interconnection 22 in the ganglions of the same name, innervate the salivary glands of the oral cavity, and the taste fibers - the papillae of the tongue, except the vallate ones. Damag to the motor nucleus or root of the facial nerve causes peripheral paralysis of the muscles of facial expression, loss of superciliary and corneal reflexes. Nerve damage at the level of the ponto-cerebellar angle is combined with damage to the vestibulo-cochlear nerve and is accompanied by taste impairment in the anterior 2/3 of the tongue, dry eyes and oral mucosa, and loss of hearing on the side of the lesion. If the nerve is affected in the facial canal below to the origin of the VIII pair, but above the origin of the greater petrosal nerve, then along with paralysis, dry eye, taste disorder, and salivation are observed. In case of nerve damage below the origin of a greater petrosal nerve, lacrimation appears due to a violation of the tone of the lacrimal sac. The damaging of the facial nerve after it leaves the skull is characterized only by paralysis of the facial muscles and lacrimation. VIII PAIR - VESTIBULO-COCHLEAR NERVE. NERVUS VESTIBULOCOCHLEARIS. AUDITORY AND VESTIBULAR PATHWAYS. Nerve of special sense, consists of two parts - cochlear and vestibular, forming the corresponding nerves, cochlear (auditory), n. cochlearis, and the vestibular (statokinetic) n. vestibularis. Cochlear nerve, n. cochlearis The first neuron of the cochlear nerve is located in the spiral ganglion, ganglion spirale (Cortii), which is placed in the spiral canal of the cochlea, canalis spiralis cochleae. Its peripheral processes go to the receptors of the organ of Corti, and central ones form the cochlear nerve. Through the floor of the internal acoustic meatus, which is adjacent to the base of the modulus, the nerve enters the internal acoustic meatus, passes through it and enters the cranial cavity through the porus acousticus internus. The nerve goes back and in the ponto-cerebellar angle, laterally to the VII pair, enters the brain, where it reaches the cochlear nuclei projecting in the lateral corner of the rhomboid fossa. There are two nuclei of the cochlear nerve: nucleus cochlearis ventralis et dorsalis, which are the the II neurons of the auditory pathway. The fibers of the dorsal nucleus make a complete decussation, forming striae medullares ventriculi quarti, and then go as part of the lateral lemniscus, lemniscus lateralis. Fibers coming from the ventral nucleus are interrupted in the nucleus of the trapezoid body of pons on its own and mainly the opposite side. For these fibers, the nucleus of the trapezoid body will be the III neuron of the auditory pathway and its processes attach to the lateral lemniscus of the opposite side. The lateral lemniscus is a continuation of the trapezoid body and its fibers go to the subcortical centers of hearing - the medial geniculate bodies, corpus geniculatum mediale, and the inferior colliculi of the midbrain, colliculus inferior tecti mesencephali. The third subcortical center is the median nucleus of the thalamus, associated with the subcortical sensory center of the extrapyramidal system. Fibers from the nuclei of the medial geniculate bodies pass through the posterior limb of the internal capsule, forming acoustic radiations, radiatio acustica, go to the cortical end of the auditory analyzer, which is located in the middle part of the superior temporal gyrus, gyrus temporalis superior, in the depths of the Silvian sulcus, in the secondary gyri of Heschl (transverse temporal gyri). Axons of the inferior colliculi form the tecto-nuclear and tecto-spinal tracts, which travel to the motor nuclei of cranial nerves and anterior horns of the spinal cord. Vestibular nerve, nervus vestibularis A nerve of special sense, conducts impulses that give information about the position and movement of the body in space. The first neuron is located in the vestibular ganglion, which is located in the floor of the internal acoustic meatus. Dendrites pass through foramens in the floor of the acoustic meatus and in the bony labyrinth. After this they follow the receptors located in the ampullary crests of the semicircular canals and in the spots of the utriculus and sacculus on the vestible of the labyrinth of the internal ear, forming the anterior, posterior, and lateral ampul23 lar nerves, nn. ampullares anterior, posterior et lateralis, saccular nerve, n. saccularis, utricular nerve, n. utricularis. Axons of the cells of the vestibular ganglion form the vestibular nerve, which goes along the internal acoustic meatus, through the porus acusticus internus penetrates the cranial cavity, enters the brain with n. cochlearis, laterally to n. facialis and ends on four nuclei projecting in the lateral corner of the rhomboid fossa, recessus lateralis or area vestibularis. The nuclei are called: 1. The superior vestibular nucleus, nucl. vestibularis superior (Bekhterev). 2. Lateral vestibular nucleus, nucl. vestibularis lateralis (Deiters). 3. The medial vestibular nucleus nucleus, nucl. vestibularis medialis (Schwalbe). 4. The inferior vestibular nucleus, nucl. vestibularis inferior (Roller). These cells are the second neurons of the vestibular nerve. Ascending fibers end on the cells of the upper nucleus, descending - on the other three. Axons of the cells of the vestibular nuclei form several bundles that are sent to the spinal cord (tr. vestibulo-spinalis), to the cerebellum (tr. vestibulo-cerebellaris), to the posterior and medial longitudinal fasciculi (fasciculus longitudinalis posterior et medialis), as well as to the thalamus (tr. vestibulo-thalamicus), followed by a continuation to the cortical end of vestibular analyzer. The processes of the second neurons go via the inferior cerebellar peduncles to nucl. fastigii of cerebellum, which will be the third neuron of the vestibular tract, which ends in the cortex of the cerebellar vermis. The other part of the fibers of lateral and medial nuclei pass through the thalamus and the posterior limb of the internal capsule and ends the cortical end of the vestibular analyzer, which is located in the middle and inferior temporal gyrus, gyrus temporalis medius et inferior. The inferior nucleus fibers forms tractus vestibulospinalis, which runs in the anterior funiculi of the spinal cord till the lowest segments of the spinal cord, and terminates on motor nuclei. As a result of a partial decusstaion of the auditory tract in the brainstem, a unilateral damage to the auditory pathway above the brainstem does not cause hearing impairment, since the function is completely compensated by the opposite hemisphere. The defeat of the auditory tract below the brainstem is accompanied by either a decrease in hearing - hypacusia, or its complete loss - anacusia. With damage to the vestibular nerve, there are disorders of orientation in space, balance, coordination of movements since communication with the cerebellum is broken, nystagmus with the nuclei of the oculomotor nerves, dizziness, vomiting - the influence of the vagus nerve. These disorders can be the result of diseases of the inner ear, pathology in the ponto-cerebellar angle, brainstem, cerebellum and cerebral cortex. It should be noted that as a result of training, addiction to vestibular irritations occurs. IX PAIR - GLOSSOPHARYNGEAL NERVE, NERVUS GLOSSOPHARYNGEUS Mixed nerve, contains motor, sensory and parasympathetic fibers. It has three nuclei located in the medulla oblongata and projecting into the rhomboid fossa in the region of the vagus nerve triangle: - motor, nucleus ambiguus, nucleus ambiguus, common with X and XI pairs; - parasympathetic, inferior salivatory nucleus, nucleus salivatorius inferior; - sensory, nucleus of solitary tract, nucleus tractus solitarii, common with VII and X pairs of cranial nerves. The nerve exits the brain in the upper part of the posterior lateral sulcus of the medulla oblongata. The nerve exits from the skull through the jugular foramen. There is a superior sensory ganglion of glossopharyngeal nerve here. Then the nerve goes to the inferior surface of the temporal pyramid, where there is an inferior sensory ganglion in the fossula petrosa. After that, the trunk of the glossopharyngeal nerve is located behind the internal carotid artery, curving in an arc, goes along the lateral edge of the stylopharyngeal muscle to the root and dorsum of the tongue, where it ends. Thus, sensory nerve fibers are represented by peripheral processes of pseudounipolar cells of the superior and inferior ganglions, the central processes of which end on 24 the nucleus of solitary tract. The motor fibers are axons of the cells of the nucleus ambiguus, and parasympathetic fibers come from the inferior salivatory nucleus. On its way, the nerve gives off branches: 1. Tympanic nerve, n. tympanicus - leaves under the inferior ganglion, consists of sensory and parasympathetic fibers, goes through the canaliculus tympanicus into the tympanic cavity, where it forms the tympanic plexus, plexus tympanicus, which together with the sympathetic fibers, from the internal carotid plexus, nn. caroticotympanici, innervates the mucosa of the tympanic cavity and auditory tube. From this plexus, a parasympathetic lesser petrosal nerve, n. petrosus minor, emerging from the tympanic cavity through hiatus canalis nervi petrosi minoris. From the skull, this nerve exits through fissura sphenopetrosa, and reaches the otic ganglion. Postganglionic branches as a component of auriculo-temporal nerve of the fifth pair are directed to the parotid gland. The whole path, including the tympanic nerve, tympanic plexus and the lesser petrosal nerve, is called the Jacobson anastomosis. 2. Pharyngeal branches, rr. pharyngei - together with the laryngeal-pharyngeal branches from the superior cervical ganglion of the sympathetic trunk and the same branches of the vagus nerve, participate in the formation of the plexus pharyngeus. 3. Tonsillar branches, rr. tonsillares - innervate the mucous membrane of the palatine tonsil and palatine arches. 4. Branch to stylopharyngeal muscle, r. stylopharyngeus - motor, innervates the muscle of the same name. 5. Lingual branches, rr. linguales - their sensory part innervates the mucous membrane of the posterior third of the tongue, taste fibers innervate the vallate papillae, and parasympathetic fibers - the small salivary glands of the tongue. 6. Sinus branch, r. sinus carotici (Hering's nerve), innervates the carotid sinus and carotid body (glomus caroticus) of the sinocarotid zone in the area of bifurcation of the common carotid artery. 7. Communicating branch with the auricular branch of the vagus nerve, r. communicans cum r. auricularis n. vagi, is involved in the innervation of the skin of the external acoustic meatus. So, the glossopharyngeal nerve provides the general and taste sensory innervation to mucous of the posterior third of the tongue, sensory to mucous of the pharynx, palatine arches, tonsils, tympanic cavity, auditory tube, external acoustic meatus, sinocarotid zone. The motor innervation is to stylopharyngeal muscle and the parasympathetic (secretory) – to parotid gland. With the defeat of this nerve, the following symptom complex is observed: 1. Loss of taste on the side of the same name on the back third of the tongue - ageusia. 2. Minor swallowing disorder, as of greater importance in the innervation of the pharynx is the vagus nerve. 3. Anesthesia of the mucous membrane of the upper half of the pharynx. Unilateral deactivation of the function of the parotid gland does not lead to dry mouth due to the compensating effect of the remaining salivary glands. X PAIR – VAGUS NERVE, NERVUS VAGUS The longest of cranial nerves. The nerve is mixed, consists of motor, sensory and parasympathetic fibers. It has three nuclei projecting in the lower triangle of the rhomboid fossa, i.e. in the medulla oblongata: - motor ambiguus nucleus, nucl. ambiguus, common for IX, X and XI pairs of cranial nerves; - sensory nucleus of solitary tract, nucl. tractus solitarii, common for VII, IX and X pairs; - parasympathetic posterior (dorsal) nucleus, nucl. dorsalis nervi vagi. From the brain, the nerve exits through the posterior lateral groove of the medulla oblongata with 5-6 roots, which are then combined into one trunk and through the foramen jugulare leaves the cranial cavity. In the jugular foramen there is a thickening - a superior sensory gangli25 on, g. superius. 1-1.5 cm inferiorly is the inferior sensory ganglion, g. inferius. Both ganglions consist of sensory cells, the processes of which make up the sensory portion of the nerve. The central processes are directed to the brain (to the sensory nuclei), and peripheral - to the periphery, as part of the branches of the vagus nerve. Then the nerve goes to the neck as part of the neurovascular bundle, consisting of the carotid artery, internal jugular vein and vagus nerve. All of them are covered with a connective tissue membrane and are located first on the side of the larynx, then on the side of the thyroid gland and trachea. When passing into the thoracic cavity, the right vagus nerve passes in front of the right subclavian artery, and the left along the anterior surface of the aortic arch. Both nerves in the thoracic cavity deviate posteriorly, go along the posterior surface of the root of the lung, and in the posterior mediastinum reach the esophagus. The right vagus nerve goes along the posterior surface of the esophagus and forms the posterior esophageal plexus there, and the left goes to the anterior surface and forms the anterior esophageal plexus, respectively. These plexuses stretch along the esophagus and pass through the diaphragm to form the anterior and posterior vagal trunks, truncus vagalis anterius et posterius. In the abdominal cavity, the anterior trunk goes along the anterior surface of the cardiac part of the stomach and breaks up into separate branches, some of them go to the liver, the rest form the anterior gastric plexus, plexus gastricus anterius. The posterior trunk goes along the posterior surface of the stomach, gives a small number of branches to its walls, and the rest of the most branches goes to the coeliac (solar) plexus, plexus coeliacus seu solaris, and is involved in its formation. The gastric branches of vagus nerve innervate the muscles, glands, and gastric mucosa. From the coeliac plexus, vegetative fibers travel through the blood vessels to all organs of the abdominal cavity, with the exception of the lower parts of the colon (descending colon and sigmoid) and pelvic organs and innervate them. Along the large vessels, a whole series of plexuses are formed. Topographically, the entire trunk of the vagus nerve is divided into 4 parts: 1. Cranial - between the superior and inferior sensory ganglions. 2. Cervical - between the inferior sensory ganglion and the origin of the recurrent laryngeal nerve. 3. Thoracic - from the origin of the recurrent laryngeal nerve to the diaphragm. 4. Abdominal - from the diaphragm to the entrance to the lesser pelvis. Branches of the vagus nerve. Cranial part: 1. Meningeal branch, r. meningeus, originating from the superior ganglion, goes through the jugular foramen into the cranial cavity and innervates the dura mater of the posterior cranial fossa. 2. Auricular branch, r. auricularis, departs from the superior ganglion, enters the jugular foramen and penetrates into the tympanic cavity through the canaliculus mastoideus, then leaves it through the tympanomastoid fissure, reaches the posterior wall of the external acoustic meatus and innervates it (which is why with irritation of the skin of the external acoustic meatus appears cough) and the skin of the external surface of the auricle. Cervical part: 1. Inferior anastomosis, r. communicans inferior, - connects the inferior sensory ganglion of the vagus nerve with the superior cervical sympathetic ganglion. 2. Communicating branch with the XII pair, r. communicans cum n. hypoglosso. 3. Superior laryngeal nerve, n. laryngeus superior, - goes to the lateral wall of the larynx and is divided into two branches - external and internal. The external branch is predominantly motor and innervates m. cricothyroideus et m. constrictor pharyngis inferior. The internal branch is sensory, enters the laryngeal cavity through the thyrohyoid membrane and innervates the laryngeal mucosa above the glottis, epiglottis and root of the tongue. 4. Pharyngeal branches, rr. pharyngei, - go to the posterior pharyngeal wall and in the region of the m. constrictor pharyngis medius, are involved in the formation of the pharyngeal 26 plexus, plexus pharyngeus. From it fibers go to the muscles of the pharynx, mucosa and muscles of the soft palate except m. tensor veli palatini, which is innervated by V pair. 5. Superior cervical cardiac branches, rr. Cardiac cervicales superiores, - contain sensory and parasympathetic fibers, pass to the heart along the wall of the common carotid artery, where they become part of the deep cardiac plexus, plexus cardiacus profundus. 6. Recurrent laryngeal nerve, n. laringeus recurrens, the right one arise from the vagus nerve at the level of the inferior margin of the right subclavian artery and rises up its posterior surface, and the left one starts at the level of the inferior margin of the aortic arch and goes back up to its posterior surface. Then both nerves go in the groove between the trachea and esophagus and reach the larynx. The recurrent laryngeal nerve contains sensory, motor and parasympathetic fibers and gives the following branches: - inferior cervical cardiac branches, rr. cardiaci cervicales inferiores, go to the superficial cardiac plexus, connecting with the branches of the sympathetic trunk; - tracheal branches, rr. tracheales - innervate the trachea (mucous membrane, glands, smooth muscles); - esophageal branches, rr. oesophagei - innervate the mucous membrane of the esophagus, glands and muscles; - inferior laryngeal nerve, n. laryngeus inferior, the final branch of the recurrent laryngeal nerve, in the larynx region breaks up into branches that innervate: all the muscles of the larynx, except for the cricothyroid, the mucous membrane of the larynx below the glottis, as well as the thyroid, parathyroid glands, thymus and lymph nodes of the neck. Thoracic part: 1. Bronchial branches, rr. bronchiales, form the bronchial and then pulmonary plexus, plexus pulmonalis, innervate the smooth muscles and glands of the bronchi and carry out the sensory innervation of the bronchi and lungs. 2. Tracheal branches, rr. tracheales, - innervate the trachea. 3. Esophageal branches, rr.oesophagei, - form the anterior and posterior esophageal plexuses. 4. Pericardial branches, rr. pericardici, - are sent to the pericardium and innervate it. 5. Thoracic heart branches, rr. cardiaci thoracici, are involved in the formation of cardiac plexuses. Abdominal part: 1. Anterior vagal trunk, truncus vagalis anterior, it gives off the anterior gastric branches, rr. gastrici anteriores, and hepatic branches, rr. hepatici. 2. Posterior vagal trunk, truncus vagalis posterior, it gives off the posterior gastric branches, rr. gastrici posteriores, coeliac branches, rr. coeliaci. As part of the branches of the coeliac plexus (see above - the course of the vagus nerve), the fibers of the vagus nerves reach the abdominal organs (liver, spleen, pancreas, kidneys, small and large intestine to the descending colon), for innervation of smooth muscles, glands and mucous membranes. In case of unilateral damage to the vagus nerve, overhang of the soft palate is observed on the damage side, its immobility or lag in this half when pronouncing the sound “A”. The uvula is deviated in a healthy direction. The voice becomes hoarse due to unilateral paralysis of the vocal fold. With bilateral damage to the vagus nerve, a nasal tone of the voice is observed, pouring of liquid food through the nose due to paralysis of the soft palate. Even a complete aphonia is possible - whispering, soundless speech. Epiglottis paralysis leads to choking during eating, coughing. Possible tachycardia and respiratory depression. Complete bilateral damage to the vagus nerves leads to death due to cardiac arrest and breathing. XI PAIR - ACESSORY NERVE, NERVUS ACCESSORIUS 27 It is a motor nerve, has two motor nuclei, one cranial - nucl. ambiguus (common with IX and X pairs), is located in the medulla oblongata, the second is the spinal nucleus, nucl. spinalis nervi accessorii, which is located in the spinal cord in the six upper segments, closer to the anterior horns. Two roots come from the nuclei: 1. Cranial roots, radices craniales, - exit the brain in the lower third of the posterior lateral groove of the medulla oblongata. 2. Spinal roots, radices spinales, - exit the spinal cord between the anterior and posterior roots, rise upwards, through the foramen magnum enter the cranial cavity and, joining the cranial roots, form the trunk of the accessory nerve. The accessory nerve leaves the skull through the foramen jugulare, and is immediately divided into two branches: 1. The internal branch, ramus internus, (mainly fibers from the cranial nucleus) approaches the vagus nerve and goes into its composition. 2. The external branch, ramus externus, - goes down, at the level of the angle of the mandible, fits under m. sternocleidomastoideus, gives branches to it, then goes to m. trapezius, and innervates it. With nerve damage, peripheral paralysis of the trapezius and sternocleidomastoid muscles is observed. XII PAIR - HYPOGLOSSAL NERVE, NERVUS HYPOGLOSSUS The motor nerve has one motor nucleus, n. nervi hypoglossi, which projects in the inferior corner of the rhomboid fossa in the triangle of the hypoglossal nerve, trigonum nervi hypoglossi. From the brain, the nerve exits between the pyramid and olive of the medulla oblongata in the anterior lateral groove by 10-15 roots. From the skull, the nerve exits through the hypoglossal canal, canalis nervi hypoglossi. It goes down to the neck, located between the internal carotid artery and the internal jugular vein, then turns forward and upward, goes along the floor of the oral cavity, enters the thickness of the tongue, where it ends. On its way, the nerve gives the following branches: 1. The superior root, radix superior, departs from the nerve at the point of its bend, connects to the inferior root, radix inferior, extending from the cervical plexus (motor branch), forming a loop of the hypoglossal nerve, ansa nervi hypoglossi or a deep cervical loop, ansa cervicalis profundus. From the loop branches go to the muscles located below the hyoid bone: m. sternohyoideus, m. omohyoideus, m. sternothyroideus, m.thyrohyoideus. 2. Lingual branches, rr. lingualis, are the terminal branches of the hypoglossal nerve and innervate all the muscles of the tongue. When a nerve is damaged, peripheral paresis or paralysis of the corresponding half of the tongue develops with atrophy and thinning of the muscles. In the case of a nuclear lesion - fibrillar twitching of the muscles of the tongue can be observed. Unilateral nerve damage does not cause noticeable functional disorders due to compensatory mechanisms (interweaving of fibers) of the opposite side. However, a bilateral lesion leads to impaired speech, which becomes entangled, indistinct - dysarthria. With a complete bilateral lesion of the nerve, speech becomes impossible, the tongue is motionless, does not protrude from the mouth - anarthria. 28